Trigger Warning: Explicit mention of suicide and self-harm.
It’s to no one’s surprise that the general public is lacking in its awareness about suicide prevention, suicide warning signs, and mental health awareness. It may be that this is a product of how some conversations in our society are still labeled as too taboo to talk about openly. Stigmatization of mental health issues is an article for another time, however.
I bring up this issue because when I tell someone of the general public that I am suicidal, I get more of a nervous laugh or an ominous, “Me too!” response. Setting aside the secondary response for a whole other conversation, the nervous laughter doesn’t exactly help me. I understand that suicide is…a complicated subject matter. But when I feel suicidal, I am often not validating my own emotional experience, and thus rely on other people’s emotional experience to identify how “bad” things have gotten for me.
This is the conversation I was having with the EMT on my way to the nearest emergency room. As we’ve seen earlier in this piece, my telling a police officer I was feeling suicidal brought me to that very same gurney. Accompanying me on my trip was Emily the moth, who had snuck in for a free ride (which is not what I can say about my own trip).
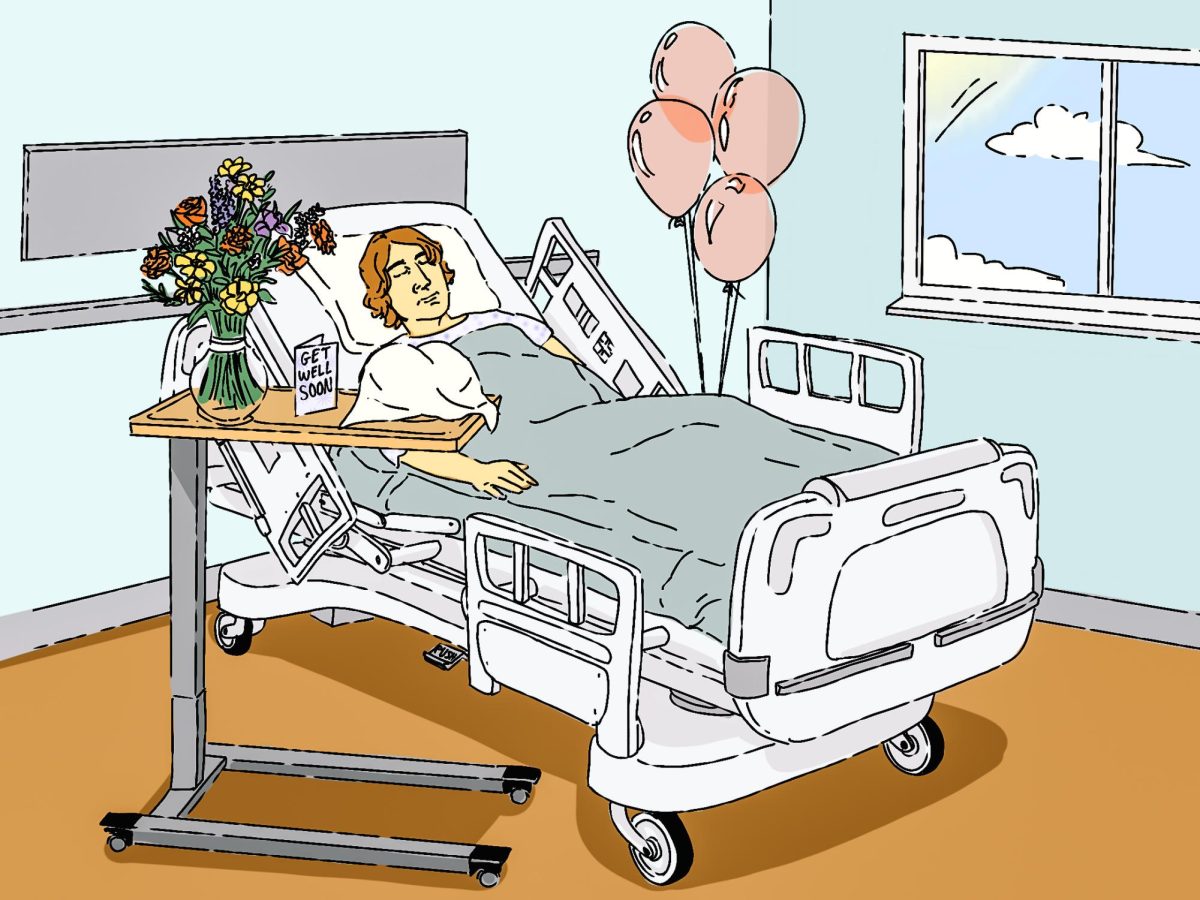
When I got to the ER, I was transferred over to what would be my “chambers” for the evening, and until 3:30 p.m. on Saturday, Sept. 17. It was a walled room, with a simple chair, a bed, blankets, and a moving table. The black object placed behind plastic turned out to be the TV, with its accompanying remote control on the wall itself. Below the TV was the window and the door itself had a window looking in as well. I read the “this room is under video surveillance” sign a good two hundred times during my stay there.
Bodily fluids were sampled, and I was to shed my civilian clothes and change into the Johnny they had there (at other times it’s been scrubs). After some time, I met with the crisis team there at the hospital. I was lucky—this woman had attended one of the International OCD Foundation conferences and was educated about OCD; she therefore understood more of what I was telling her about my own experiences.
Due to the action I had taken of speeding and my previous history of suicide attempts, it was ruled—unsurprisingly to me, although I was reluctant—that I’d be hospitalized. The next action was to wait for a bed to open up at a nearby psychiatric hospital. And so began the countdown.
Here I was, alone in a room under surveillance, a remote control for some unimpressive TV channels on the wall of my room (which meant I wasn’t getting up to turn it on), with limited staff in the evening shift, and with all the time in the world to obsess and fixate on my thoughts.
It should come as no surprise, then, that at some point the following morning I was twice as suicidal as when I had gotten in.
I got to continue texting friends up until 11 p.m., which helped until I had to hand my phone over. It was also helpful that I received a couple of loose coloring pages, a word search, and some crayons. I got to scrawl out the phone numbers of friends I could contact while in the hospital on the back of the word search page (which was a Finding Nemo one).
But once without a phone and without contact with the outside world, I was left to replay the incident with the police officer over and over in my mind. I was shrinking internally from sheer boredom. My brain would not shut up for the life of me, and over and over I thought about the ways I could hurt myself based on what was available to me in that small room. I could slam my head on the table (or the wall), I could strangle myself under the bedsheets, I could scratch myself, and so on. I spent hours thinking of this, wide awake at two in the morning until 3 a.m. when I played five questions with one of the nurses and got a melatonin (sleeping aid).
I spent most of Saturday sleeping, and some time watching “Horrible Bosses” on the television. Around seven in the morning on Saturday I cried to myself because I was so distraught from the cruel heaviness with which the OCD was lacing venom through my brain. I thought over and over about all the reasons why I should hurt myself and the idea grew more and more appealing.
I don’t even remember what manure my brain was feeding me, but I know it had to do with reasons why I should let go of my life and just kill myself. Looking back on it, there may have also been some depression at play there, too. I didn’t want to feel like I had to act on it, but I couldn’t validate myself for being serious if I was feeling suicidal and did NOT act on it. It seemed to lose its seriousness if there wasn’t any action taken. Like it didn’t matter and was “no big deal.” And it was something I had to prove to myself—I could kill myself, or attempt to, even if I didn’t want to actually die.
My brain told me that life wasn’t worth living with the OCD and I would be better off dead, without anyone to find me and no one to find out what I had done. So in response, I cried. Because there was no one around to witness my pain and to acknowledge how badly the situation sucked and how, even despite this, things would get better.
After some time, when I felt defeated and felt like the only way I could talk to someone was if I tried to hurt myself within that room, I got my breakfast tray. It was this super soggy blueberry muffin; I didn’t eat much of it because I was so disgusted with myself at that point for still being alive. My appetite from 4 a.m. had faded with the oncoming cruelty of my thoughts.
One of the staff had asked me if I’d like to speak with someone from the crisis team and I agreed that I would.
For the next hour, I waited for someone to come and talk to me. I still contemplated all the ways I could hurt myself, and arrived at the position that I’d scratch myself ever so slightly.
I never did speak to someone again during the time I was twiddling my thumbs trying to ignore the brass nature of my brain.
I did get to make a couple of phone calls, though, and that helped me out a lot. Getting to hear some of my friends’ voices really helped pull me through and have something to look forward to. One of my friends “Jeanine” would come to visit me while I was in the psychiatric hospital. That gave me the happiness and motivation to color in a Squirtle picture for her and write a little note on the back of it.
I know you may be reading this and are wondering where my point is going with all of this background information. To that, I say don’t worry; this is likely the most background information we’ll get out of this.
I wanted to set the scene properly for what my experience was like in the Emergency Room and how it may reflect other people’s experiences in a negative light. I’m saying it because it needs to be said, it needs to be known, and it needs to be addressed.
I will always recommend the Emergency Room for someone who is struggling with suicidal thoughts. If you are suicidal and you think you may act on it, you NEED to go to the hospital. You NEED to keep yourself safe, and the safest place you can be is at a place where you’re able to rehabilitate until you feel better—which will be approximately a week later. Granted, you may not exactly feel like yourself again once you get out of the hospital, but it’s highly likely that the suicidal crisis will have passed. Another may arrive, but that’s beside the point.
I do not want the takeaway of this storytelling to be that the Emergency Room is always a cruddy space and for that to be a reason someone decides against their better judgment to not go.
Sometimes the emergency room is a cruddy experience. But the ER is the place you go to before you get to the treatment facility. It’s the annoying step in between.
I want to make suggestions on how to improve the quality of an ER visit for psychiatric issues, rather than discourage people from attending them if they need it.
For one, advocating for yourself is huge. Ask for crayons and some coloring sheets. Or if you’re able, and you know you’re going to the hospital, bring a book to read.
Write out a list of phone numbers of friends and family that you can contact during your stay within the ER and the psychiatric hospital. Having social support is a HUGE part of recovery, and it’s nice to get to see some familiar faces who know the real you and not just the disorder you’re struggling with.
If you’re able to, have someone accompany you to the ER, whether that’s a friend or a family member. This will stave off some of the boredom and sheer emotional weight that you may experience while staying in the ER. I know in my first hospitalization, I had my father with me in the ER, and that helped out a lot, compared to the times when I was alone.
If you’re able to plan even a little bit ahead for your hospitalization, I recommend bringing some type of backpack with some books to read, coloring utensils, and coloring books, as well as some clothes (without strings) for when you get to the psychiatric hospital. They’ll keep your stuff away from you and it’ll come with you during transport but at least you’ll have some clothes to change into when you get to the psych hospital.
I also recommend bringing something that reminds you of better times—for instance, I brought my stuffed animal with me while I was in the psychiatric hospital because it was something physical for me to hold onto.
Additionally, as I’m writing this within October 2016, I have come to find out that only 30 states in the US offer legally recognized mental health directives, although Massachusetts is not one of them. However, there exists a mental health directive that you can use as a working template that covers multiple facets involving what medications you’re taking, your treatment providers and their contact information, someone they can contact to vouch for you, and more. It isn’t legally binding, but it’s a resource. If you can’t find it online, you can try and track me down and I can make a copy of it for you.
Lastly, referring back to the first tip: advocate, advocate, advocate. I’m not the type to lash out when my treatment isn’t being respected or I really, really want to get out of the hospital. I know from seeing others practice such behaviors that it only makes the situation worse. However, I absolutely hate and loathe that I felt in my ER visit that the only way I could receive help there via talking to someone is if I acted out. I did not act out and I did not see that crisis team personnel. I wish I could say that I did, but it just wasn’t the case for me.
My tip is to be patient, be compassionate, and be persistent. If you feel unsafe, tell someone. Before you act on the thought, tell someone. This is true even outside of the hospital. The length of your ER visit depends on when the nearest psychiatric bed is open. I’ve had the process take from five hours to as long as the next day at times. If you can talk to someone who knows the good places to go to versus the not so great ones, utilize that information to create a list of places you can refer to if you ever land in a hospitalization setting.
Remember, though, that the ER stay is time-limited. Eventually, you will get to the real part of treatment, which lies within the psychiatric hospital or psychiatric ward. Just keep breathing, safety contract for five minutes and soon you’ll be out of there.
Stay safe, people.
Inside A Psychiatric Hospitalization II
October 17, 2016